Notice:
We are supporting members and providers impacted by the tragic flooding in Washington state. Click here to learn more.
Delta Dental of Washington Individual and Family Dental Plans
We offer a variety of Individual and Family dental plans for patients both on and off the Washington Health Benefit Exchange (WAHBE).
Our Individual and Family plans are administered by Wyssta Services, Inc.. As our Health Care Benefit Manager, Wyssta Services, Inc. performs certain tasks on Delta Dental of Washington’s behalf, such as enrollment, claims processing, and customer service. For more information regarding the role of a health care benefit manager, click here.
Washington Health Benefit Exchange (WAHBE) Plans
The Washington Health Benefit Exchange (WAHBE) is a provision of the Affordable Care Act and provides a marketplace for dental and health insurance for individuals and families in Washington State. We're proud to partner with WAHBE in providing dental benefit plans for qualifying families and kids. Patients may search for plans and enroll by visiting https://www.deltadentalwa.com/our-plans/wahbe.
Important: Claim payment may be delayed for delinquent premium payment
The Washington Health Benefit Exchange does not require subscribers to pay their premium at time of enrollment and all plans offered on WAHBE have a federally mandated grace
period of 30 days for the premium to be paid by the insured.
Delta Dental of Washington will hold claims until we receive premium payment. If no premium payment is made, all pending claims will be denied, and the patient will then be fully responsible for any
claims.
Our experience shows this has the potential to affect a significant number of claims, so it's important that you're aware. When checking eligibility through our website, the Interactive Voice Response (IVR) system or your practice management system, the
patient will show as eligible during this grace period. As the grace period is a federally mandated requirement, any late charge interest normally considered for a delay in processing a clean claim will not be paid.
Important documents and resources
2. Orthodontic medical necessity form
Downloadable PDF
Plans for Individuals and Families available off WAHBE (Delta Dental Covers Me Plans)i
We offer plans for patients outside of the Washington Health Benefit Exchange. Coverage is available to all permanent residents in Washington State. Individual plans are designed for anybody who does not have dental coverage through their current employer or would like additional dental coverage for themselves or their family. Patients can learn more about our plans and enroll by visiting https://www.deltadentalwa.com/our-plans/dental/ and clicking “Get Quote”.
|
Our highest annual maximum, and three periodontal maintenance cleanings per year |
Orthodontic benefits such as braces and aligners installed by DMD or DDS |
No waiting period and coverage that increases over the first two years you renew |
100% coverage on most preventive care services and 50% on most major procedures |
Most affordable plan that covers preventive care, fillings, and non-surgical extractions |
|
|---|---|---|---|---|---|
|
Monthly Premium Eastern WA |
$68.15ii |
$63.45ii |
$60.55ii |
$56.50ii |
$33.95ii |
|
Monthly Premium Western WA |
$78.30ii |
$72.90ii |
$69.60ii |
$65.00ii |
$39.10ii |
|
Plan Year Maximum |
$2000 |
$1500 |
1st Yr, 2nd Yr, 3rd Yr |
$1000 |
$1000 |
|
|
None |
$250 per person up to $1250 |
None |
None |
None |
|
Deductible |
$100 |
$50 |
$50 |
$50 |
None |
|
Office Visit Copay |
None |
None |
None |
None |
$15 |
|
Preventive Care |
100% |
100% |
100% |
100% |
100% cleanings and exams |
|
Fillings |
80% |
50% |
1st Yr, 2nd Yr, 3rd Yr |
50% |
50%iv |
|
Crowns |
50%v |
50%v |
50%v |
50%v |
Not Covered |
|
Root Canal |
50% |
50% |
50% |
50% |
Not Covered |
|
Implants |
50% |
50% |
50% |
50% |
Not Covered |
|
Non-Surgical Extractions |
50% |
50% |
50% |
50% |
50% |
|
Surgical Extractions |
50% |
50% |
Not Covered |
Not Covered |
Not Covered |
|
Periodontal Maintenance |
50%viii |
50% |
1st Yr, 2nd Yr, 3rd Yr |
50% |
Not Covered |
|
Orthodontics |
Not Covered |
50%ix |
Not Covered |
Not Covered |
Not Covered |
|
Annual Contract |
Yes |
Yes |
Yes |
Yes |
Yes |
|
Waiting Period |
May Apply |
May Applyxi |
None |
May Apply |
May Apply |
Coverage percentages displayed in the table above represent the percentage of the allowed amount that is covered by Delta Dental of Washington.
i. These are benefit highlights only. Monthly premiums shown are examples of monthly rates for subscriber-only in Washington, effective January 2026. Actual rates may vary (higher or lower) based on plan effective date, plan choice, your age, your location, number of people insured, their age, and relationship to you. For full details of plan, benefits, and pricing, please visit DeltaDentalCoversMe.com.
ii. Individual 12-month contracted rate.
iv. Excludes back teeth tooth-colored fillings.
v. A pretreament estimate is suggested. Clinical requirements must be met, crowns covered at 50% per tooth every seven years.
viii. No waiting period.
ix. $1500 lifetime maximum with 12-month waiting period.
xi. For Orthodontia-covered procedures, a 12-month waiting period applies. This means that DDWA will not pay towards any of these procedures until the covered members have been enrolled in this policy for 12 continuous months. The waiting period for Orthodontia treatment will be waived for your family if all family members were covered under another insured dental plan with orthodontic coverage for at least 12 continuous months before you enrolled in this plan, but only if there was no more than a 63-day gap between the previous plan and this plan. Documentation is required to waive the 12-month waiting period.
2026 Individual and Family Plan Policies
Delta Dental – Optimum Plan
Downloadable PDF
Delta Dental – Premium Plan
Downloadable PDF
Delta Dental – Plus Ortho Plan
Downloadable PDF
Delta Dental – Ascent Plan
Downloadable PDF
Delta Dental – Enhanced Plan
Downloadable PDF
Delta Dental – Clear Plan
Downloadable PDF
Delta Dental – Basic Plan
Downloadable PDF
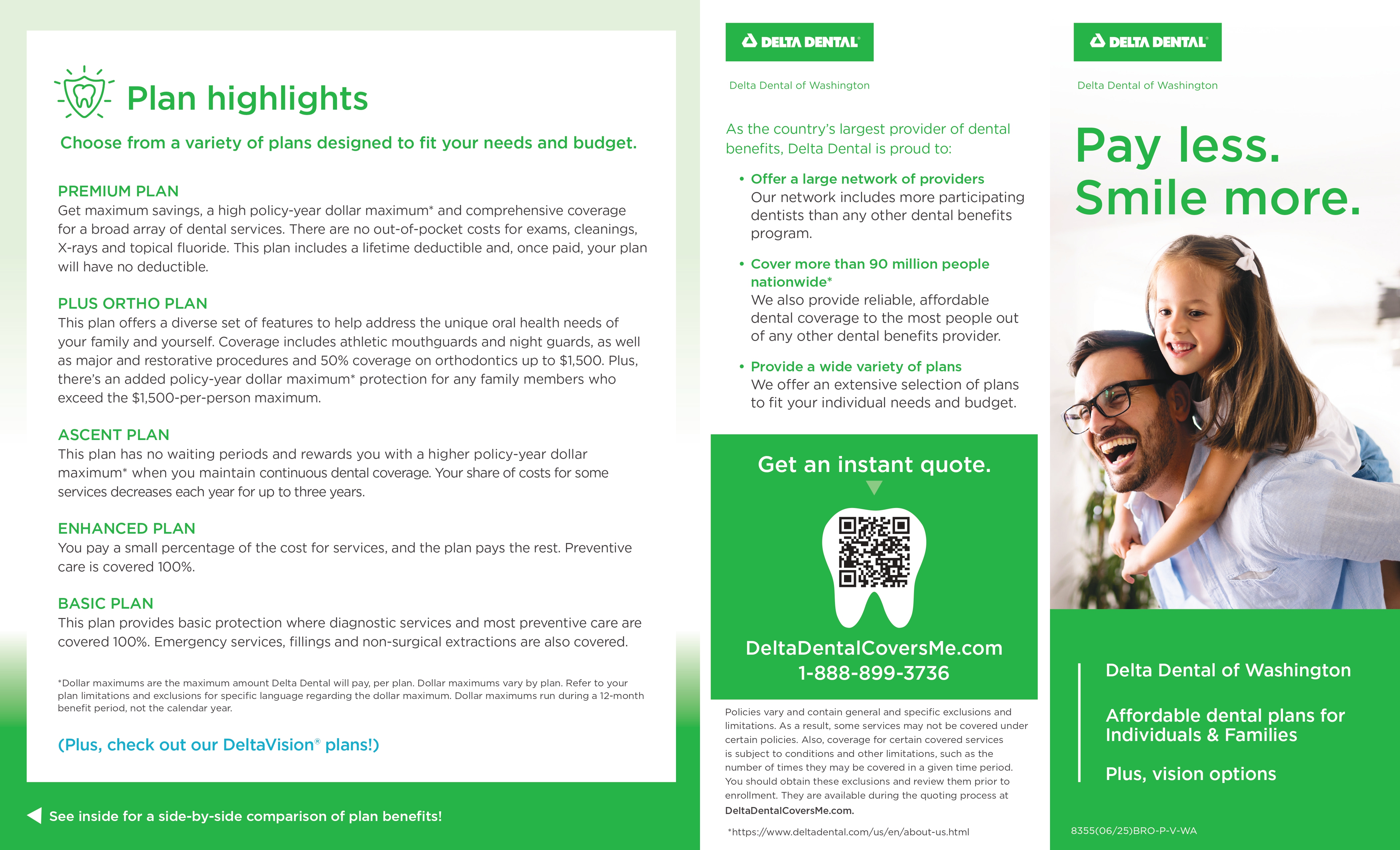
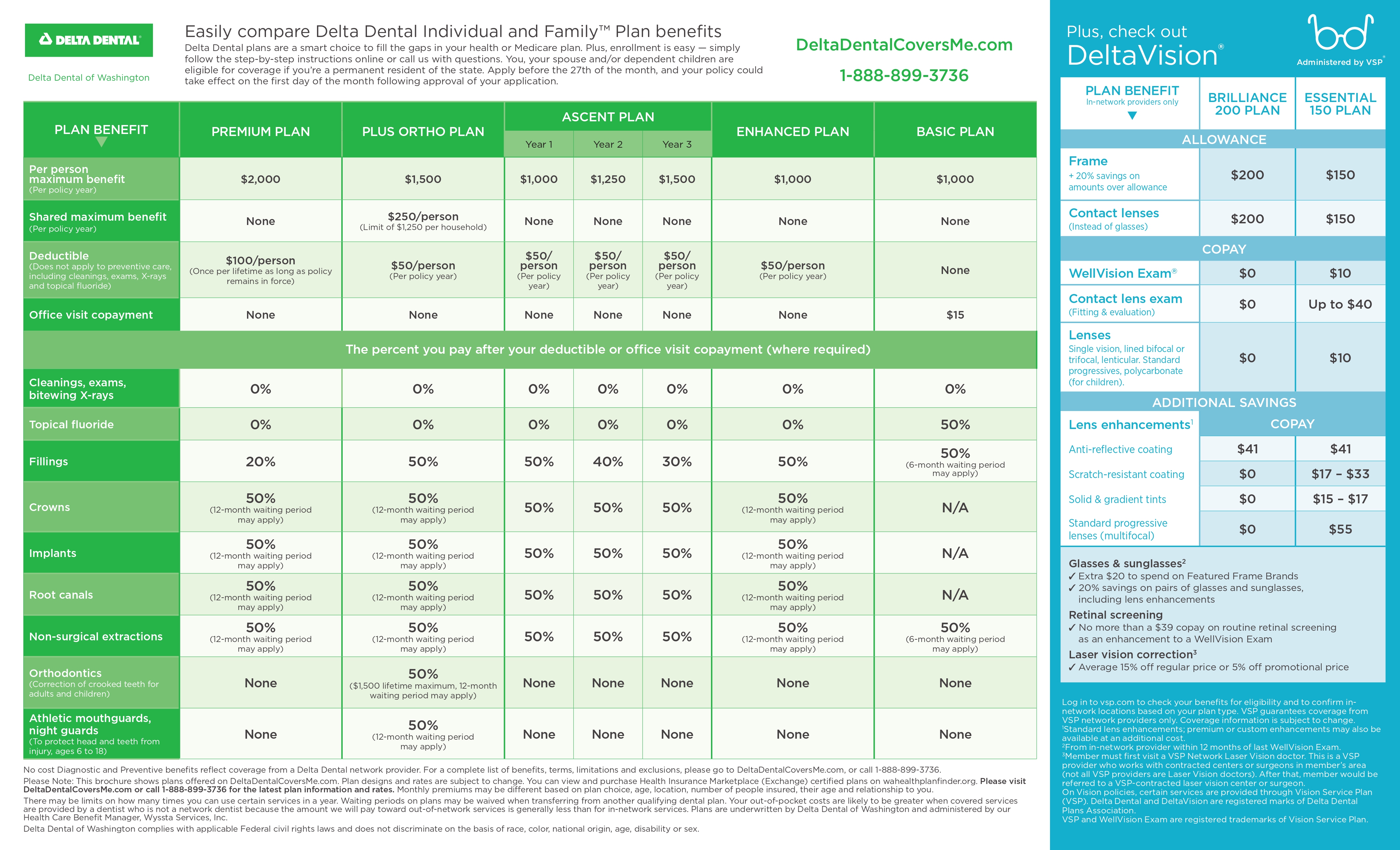
Free Office Materials
With health care and health insurance top-of-mind, more patients than ever may be asking your office for recommendations on dental coverage. We’re happy to provide you with easel displays and brochures featuring our Delta Dental Covers Me Individual & Family plans available off
WAHBE.
To order materials for your office, call us at 1-844-759-6020 or visit us online at http://www.reorder.rgcnet.com/
Easel Display
Brochure Example
Front
Back
Contact Information
For questions and more information about Individual and Family Plans, please call Wyssta Services, Inc. at 1-888-899-3734 M-F, 8 a.m. to 5 p.m or refer to the Delta Dental Covers Me provider portal at https://my.deltadentalcoversme.com/provider.
Frequently Asked Questions
I see that some plans state, “waiting period may apply.” What does this mean?
Certain policies have a 12-month Waiting Period that applies to certain covered procedures. This means that Delta Dental of Washington will not pay towards any of these procedures until the patient has been enrolled in this Policy for 12 continuous months. Please see the “Benefits” section of the specific policy document for procedures that are subject to the Waiting Period. Any Waiting Periods will be waived for your patient if they were covered under any other dental plan(s) for at least 12 continuous months before they enrolled in this Plan, and only if there was no more than a 63-day gap between your patient’s previous policies and this Policy. Your patient will need to supply information about their previous plans to make sure they qualify for a Waiting Period waiver. Waiting Periods will not be waived for new members added to this Policy without prior qualifying coverage, or if there was more than a 63-day gap between any of their previous Policies and the effective date of this Policy.
I can’t find information on the missing tooth clause.
There is no missing tooth clause.
Details regarding prosthetic appliances used to replace missing teeth:
- The appliance may be a partial denture, full denture, implant and implant related procedure, or a fixed bridge.
- Replacement of an existing appliance is covered once every seven years and only when it cannot be repaired
- Covered only for persons ages 16 years and older

